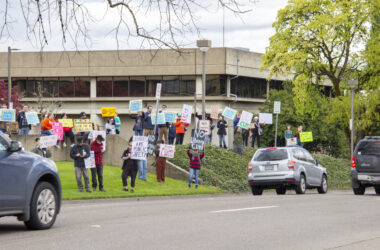
The Marion County Health and Human Services headquarters in Salem (Rachel Alexander/Salem Reporter)
The Marion County Health and Human Services headquarters in Salem (Rachel Alexander/Salem Reporter)
As Oregon has confirmed more cases of the novel coronavirus, readers have lots of questions about the state and local response, how the virus is spread and why certain health measures are or aren’t being taken.
This is designed to answer the most common questions and will be updated as the outbreak evolves and as more information becomes available. If you want to submit additional questions, send them by email to [email protected].
Last updated March 11, 2020 at 10:15am with specific numbers for Salem Hospital capacity.
What do we know about the Marion County case of the novel coronavirus? Why don’t we know more?
As of Tuesday, March 10, Marion County has one presumptive positive case of the novel coronavirus. A presumptive diagnosis means the state health laboratory has determined through testing that the person is presumed to have COVID-19 but the federal Centers for Disease Control and Prevention hasn’t provided a confirming diagnosis.
State and county health officials announced the case at a March 8 news conference and said it was a case of community spread. The sick person has not had contact with other confirmed cases or traveled to a place where the infection is widespread.
Oregon Health Authority leaders have kept a tight hold on other information about cases, asking county health departments not to share information. They are sharing some information on a statewide level about patient ages and how many have been hospitalized.
Salem Reporter requested from Marion County officials the patient’s age range, sex, how serious the patient’s illness is and whether and where the patient is receiving care. Marion County public health administrator Katrina Rothenberger and spokeswoman Jolene Kelley declined to answer all those questions, citing guidelines from the state and patient confidentiality.
Where in Marion County does the patient live?
Health officials won’t say.
A Johns Hopkins University team is mapping all cases of the disease worldwide, including in Marion County. The dots on that map display a random location within the affected county, Marion County spokeswoman Jolene Kelley said. The location of the dot in Marion County does not indicate the patient is at that particular location, though the county has been getting questions about the map.
What happens when someone tests positive for the virus in Oregon?
State workers notify county health officials when a person in their county tests positive.
County health workers then interview the patient to determine others who might be at risk of infection based on close contact with the patient.
When that “trace investigation” identifies people at risk, a county health worker will call, explain the circumstance, and asked that they voluntarily quarantine themselves for 14 days after their last contact with the person. That period is thought to be the longest someone could be infected without showing symptoms. Health workers stay in contact with people during isolation to see if they develop symptoms.
So far, Marion County officials said everyone they’ve identified who has had contact with the first identified case has agreed to quarantine themselves, typically at home.
Why aren’t health officials saying where people with the disease have been?
In past disease outbreaks in Oregon, local and state authorities have shared public locations where people ill with a disease have been so they can identify people likely at risk for infection. That was the case during a 2019 measles outbreak in Oregon and Washington.
They’re not doing that for coronavirus because of differences in how the disease spreads, said Katrina Rothenberger, Marion County’s public health administrator. She also cited patient confidentiality.
COVID-19 is mostly spread through direct person-to-person contact, usually through being close to an infected person who’s coughing. Those considered in “close contact” with a confirmed case are at risk. “Close contact” is more than being in the same room with a patient – it means being within about six feet, or having an infected person cough or sneeze on you.
People can ingest the virus by touching a contaminated service and then touching their face, though the CDC and World Health Organization say that’s not the primary way the virus is spreading. Health officials recommend regular cleaning of surfaces that may have been exposed. It’s not yet known how long the virus can live on surfaces, but soap, bleach and other common household cleaners are effective in killing it, according to the WHO.
How will we know if a local school is impacted?
State officials are informing school districts if a student or employee tests positive for the disease and sharing that information publicly.
Salem-Keizer school district spokeswoman Lillian Govus said March 9 that they haven’t received any notice related to the single Marion County case, so the patient is not a student or school employee.
The flu kills more people than the novel coronavirus. Why is everyone so concerned about this virus?
Scientists and public health officials have given three main reasons for concern about COVID-19: it’s unknown, it appears significantly more fatal than the flu for those who are infected, and it could overwhelm healthcare facilities.
Tens of thousands of Americans do die annually from the flu, but seasonal influenza is also far more widespread. The percentage of people who get the illness and die (known as the case-fatality rate) is below 0.1%, according to the World Health Organization.
It’s hard to say what the true fatality rate for COVID-19 is yet because data is still being collected. Globally, 3.4% of people with confirmed COVID-19 cases have died as of March 6, according to WHO data. Chinese health data suggests a much higher death rate of 14.8% for those over 80.
Health providers are mostly aware of serious cases requiring hospitalization, which skews the fatality rate up because people with mild cases who don’t seek care aren’t included in official numbers. But there’s broad agreement among health officials that the virus is more deadly than the flu – it just hasn’t spread as far yet.
Also of concern to health providers is their ability to care for large numbers of seriously ill patients. Hospitals are typically at peak capacity during flu season, and adding more seriously ill patients who require ventilators and other equipment could strain them further, said Dr. Steve Vets, emergency room medical director at Santiam Hospital. That’s especially true if large numbers of nurses and staff are themselves quarantined.
What is Salem Health doing to prepare for more hospital cases?
Salem’s only hospital is operating normally and “closely managing” supplies of masks, gloves, gowns and other protective equipment to conserve supply for when it’s needed, according to Karl Wright, director of supply chain services. There are no shortages.
The hospital has a task force meeting daily to review the COVID-19 outbreak and manage risks and impacts to the hospital. Hospital officials said they take similar measures when the hospital is especially full, Wright said. Salem Health hospitals and clinics have had screening guidelines for suspected COVID-19 cases in place for several weeks with separate entrances and waiting areas for those suspected of having the virus.
The hospital has 48 intensive care unit-capable beds and 27 negative airflow rooms, spokesman Elijah Penner said. Negative air flow rooms draw air from the outside in and are commonly used to quarantine patients with serious respiratory illnesses in hospitals.
If the hospital does see an influx of patients, it can take steps to reduce the burden on the emergency room, Penner said, including expanding hours of outpatient care facilities, discharging patients home with follow-up care plans and using telemedicine visits and nurse triage call lines to screen patients.
Penner wouldn’t say whether the Marion County coronavirus patient is being treated at a Salem Health facility.
Why isn’t Oregon closing schools?
The Oregon Health Authority and the Oregon Department of Education currently recommend against closing schools unless a staff member or student tests positive for the virus. Even then, they suggest schools consider alternative measures before shutting down.
Oregon officials are relying on CDC guidelines developed for mild or moderate influenza outbreaks, which don’t recommend preemptive school closures.
Schools are encouraged to have students with a fever or other symptoms of the virus, like a dry cough and shortness of breath, stay home until they feel well.
State guidelines issued March. 8 cite the low number of cases of COVID-19 in children globally, and the other impacts school closures would have on students and families. Though the reasons aren’t yet well-understood, the disease is typically mild in children without underlying health conditions.
Schools are judging the potential public health benefits of closures with the impacts on students and families who rely on schools for regular meals and other resources. About 70% of Salem-Keizer’s 41,000 students qualify for free or reduced cost lunch, and local elementary schools serve about 15,000 meals per day. The district also has about 1,000 homeless students, and more who don’t have computers or internet access at home, making online classes difficult for many students.
Stores are sold out of hand sanitizer and disinfecting wipes. How can I prevent the spread of virus?
Regular hand soap is extremely effective at killing the virus. Washing your hands regularly (with hot or cold water) remains the number one step public health officials are telling healthy people to take, especially after coughing or sneezing, using the bathroom and before preparing food. Hand sanitizer with at least 60% alcohol should be used if soap and water are not available.
For cleaning surfaces, bleach, rubbing alcohol and hydrogen peroxide are all effective at killing the virus, in addition to many regular household cleaners. The CDC suggests this list as a resource.
Resources
World Health Organization frequently asked questions
Centers for Disease Control and Prevention frequently asked questions
Marion County COVID-19 updates
Oregon Health Authority COVID-19 updates
PREVIOUS COVERAGE:
As Oregon expands coronavirus testing, uninsured patients may struggle with access
What can state government do if the coronavirus outbreak gets worse?
Eight major Oregon insurers agree to waive co-pays, deductibles for COVID-19 testing
Santiam Hospital doctor reports back from caring for quarantined coronavirus patients in Nebraska
Salem-area health officials say local coronavirus cases likely a matter of when, not if
After initial stumble, Oregon prepares to ramp up testing of possible coronavirus cases
Coronavirus outbreak could affect Oregon’s economy, including exports
It’s business as usual, but with more hand sanitizer, in Salem-Keizer schools
Contact reporter Rachel Alexander at [email protected] or 503-575-1241.

Rachel Alexander is Salem Reporter’s managing editor. She joined Salem Reporter when it was founded in 2018 and covers city news, education, nonprofits and a little bit of everything else. She’s been a journalist in Oregon and Washington for a decade. Outside of work, she’s a skater and board member with Salem’s Cherry City Roller Derby and can often be found with her nose buried in a book.